The Legacy of NG59
NICE treatment guideline NG59, published on 30th November 2016 was a landmark guidance attempting to rationalise the treatment of chronic low back pain and sciatica in the over 16’s. This is a complex document which offers guidance in treatment of back pain and sciatica at 3 levels, ie self help / community, primary care and secondary care. Furthermore it offers guidance in the areas of manual therapy, pharmacotherapy (medications) and invasive therapies (injections and surgery)
This comprehensive document covers a wide range of treatments. As a pain specialist, the main areas of interest are in the pharmacotherapies and invasive therapies. The main points of interest in these areas are highlighted below
Pharmacological Interventions
The main points of interest in drug treatment of chronic low back pain in adults are highlighted below
1.2.17 Consider oral non-steroidal anti-inflammatory drugs (NSAIDs) for managing low back pain, taking into account potential differences in gastrointestinal, liver and cardio-renal toxicity, and the person’s risk factors, including age.
1.2.18 When prescribing oral NSAIDs for low back pain, think about appropriate clinical assessment, ongoing monitoring of risk factors, and the use of gastroprotective treatment.
1.2.19 Prescribe oral NSAIDs for low back pain at the lowest effective dose for the shortest possible period of time.
1.2.20 Consider weak opioids (with or without paracetamol) for managing acute low back pain only if an NSAID is contraindicated, not tolerated or has been ineffective.
1.2.21 Do not offer paracetamol alone for managing low back pain.
1.2.22 Do not routinely offer opioids for managing acute low back pain (see recommendation 1.2.20).
1.2.23 Do not offer opioids for managing chronic low back pain.
1.2.24 Do not offer selective serotonin reuptake inhibitors, serotonin–norepinephrine reuptake inhibitors or tricyclic antidepressants for managing low back pain.
1.2.25 Do not offer anticonvulsants for managing low back pain.
Invasive Treatments
1.3.1 Do not offer spinal injections for managing low back pain.
Radiofrequency denervation
1.3.2 Consider referral for assessment for radiofrequency denervation for people with chronic low back pain when:
- non-surgical treatment has not worked for them and
- the main source of pain is thought to come from structures supplied by the medial branch nerve and
- they have moderate or severe levels of localised back pain (rated as 5 or more on a visual analogue scale, or equivalent) at the time of referral.
1.3.3 Only perform radiofrequency denervation in people with chronic low back pain after a positive response to a diagnostic medial branch block.
1.3.4 Do not offer imaging for people with low back pain with specific facet join pain as a prerequisite for radiofrequency denervation.
Epidurals
1.3.5 Consider epidural injections of local anaesthetic and steroid in people with acute and severe sciatica.
1.3.6 Do not use epidural injections for neurogenic claudication in people who have central spinal canal stenosis.
Surgical Interventions
Spinal fusion
1.3.9 Do not offer spinal fusion for people with low back pain unless as part of a randomised controlled trial.
Disc replacement
1.3.10 Do not offer disc replacement in people with low back pain.
What Are the Implications of NG59 for Secondary Care?
Secondary care is when you are referred to a hospital specialist in back pain – traditionally either a surgeon to consider surgery or a pain specialist to consider specialist medications or injections.
As can be seen from the above, the recommendations of NG59 imposes quite strong limitations on what either specialist can offer, and, in fact, pushes the vast majority of adult chronic mechanical back pain sufferers back to primary care or self help, with the assistance of physiotherapy and psychological support.
Implications for Pharmacotherapy
As can be seen from above, there is quite a limited choice of drugs available for treatment of chronic low back pain. This is essentially limited to paracetamol and codeine combinations (not paracetamol alone) and short courses of non-steroidal anti-inflammatory drugs (NSAID’s) such as ibuprofen, naproxen or diclofenac. Many of the groups of drugs used for other chronic pain conditions such as opioids, tricyclic antidepressants and gabapentinoids or other anti-convulsant drugs are not recommended.
Ultimately this leaves quite a short list of drugs that can be used for chronic mechanical low back pain. These drugs can often be bought in over the counter preparations.
Implications for Invasive Therapies
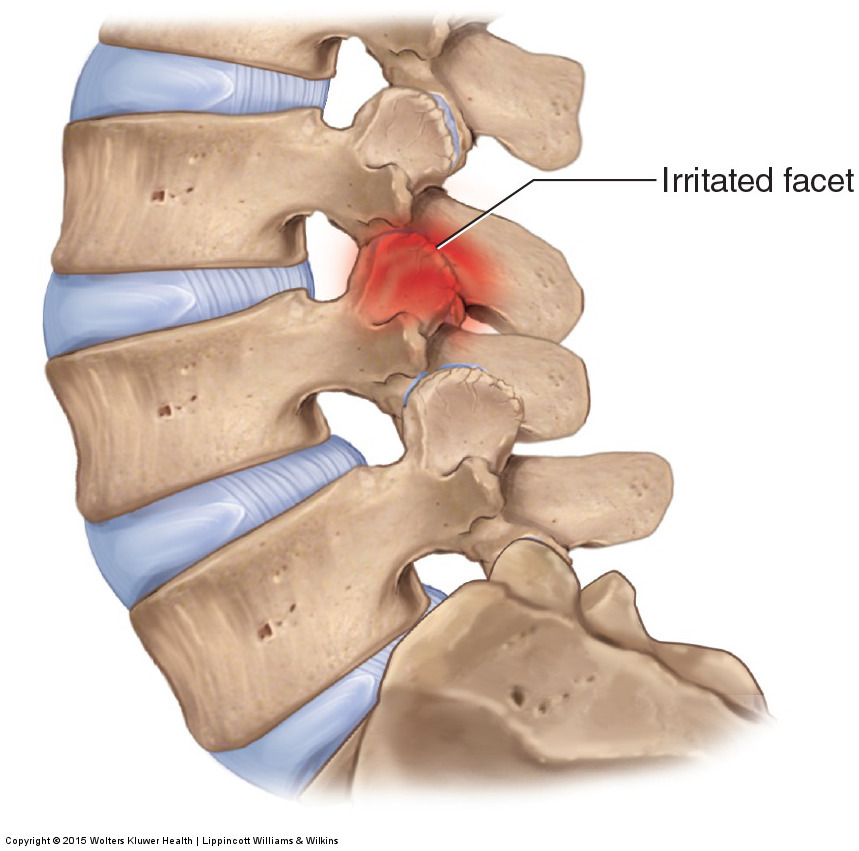
The main message regarding invasive therapies are that spinal injections and spinal surgery should not be offered for treatment of chronic low back pain. The only invasive therapy suggested is medial branch radiofrequency ablations. This currently is the treatment of choice for mechanical low back pain, but must be preceded by test / diagnostic injections called medial branch blocks, to confirm that the facet joints in question are the source of pain and as a predictor whether the radiofrequency ablation is likely to be successful.
Overall, as can be seen, the current trend in management of chronic low back pain is to move away from the specialist setting, back towards community / self help with the benefit of physiotherapy and psychological support.
The options available to a chronic pain specialist are somewhat limited, in terms of medications and injections. As can be seen, the medication options are essentially limited to simple analgesia and short courses of NSAID’s.
Radiofrequency ablation is the only invasive treatment that makes the list. Spinal injections and surgical interventions are no longer recommended. The implication of this is that spinal surgeons should not be receiving any referral for mechanical low back pain. A surgeon should only be consulted if any of the ‘red flags’ are present.


Using active rehabilitation, pain relief, and psychological support, Dr. Michael Stafford helps patients avoid surgery while improving long-term function and quality of life.